Psoriatic arthritis (also arthritis psoriatica, arthropathic psoriasis or psoriatic arthropathy) is a type of inflammatory arthritis that will develop in up to 30 percent of people who have the chronic skin condition psoriasis. Psoriatic arthritis is classified as a seronegative spondyloarthropathy and therefore occurs more commonly in patients with tissue type HLA-B27.
Signs and symptoms
- Pain, swelling, or stiffness in one or more joints is commonly present.
- Asymmetrical oligoarthritis (70%) (Involvement of the distal interphalangeal joints (DIP) is a characteristic feature).
- Sacroiliitis/spondylitis (40%)
- Symmetrical seronegative arthritis (15%)
- Distal interphalangeal joint arthritis (15%)
- Hand joints involved in psoriasis are proximal interphalangeal (PIP) + distal interphalangeal (DIP) + metacarpophalangeal (MCP) + wrist
- Joints that are red or warm to the touch.
- Sausage-like swelling in the fingers or toes, known as dactylitis.
- Pain in and around the feet and ankles, especially tendinitis in the Achilles tendon or plantar fasciitis in the sole of the foot.
- Changes to the nails, such as pitting or separation from the nail bed.
- Pain in the area of the sacrum (the lower back, above the tailbone).
- Along with the above noted pain and inflammation, there is extreme exhaustion that does not go away with adequate rest. The exhaustion may last for days or weeks without abatement. Psoriatic arthritis may remain mild, or may progress to more destructive joint disease. Periods of active disease, or flares, will typically alternate with periods of remission. In severe forms, psoriatic arthritis may progress to arthritis mutilans which on X-ray gives pencil in cup appearance.
- Because prolonged inflammation can lead to joint damage, early diagnosis and treatment to slow or prevent joint damage is recommended.
- Scaly skin lesions are seen over extensor surfaces (scalp, natal cleft and umbilicus).
- The nail changes are pitting, onycholysis, sub-ungual hyperkeratosis and horizontal ridging.
Psoriatic Arthritis Medicine Video
Causes
The exact causes are not yet known, but a number of genetic associations have been identified in a genome-wide association study of psoriasis and psoriatic arthritis including HLA-B27.
Diagnosis
There is no definitive test to diagnose psoriatic arthritis. Symptoms of psoriatic arthritis may closely resemble other diseases, including rheumatoid arthritis. A rheumatologist (a doctor specializing in diseases affecting the joints) may use physical examinations, health history, blood tests and x-rays to accurately diagnose psoriatic arthritis.
Factors that contribute to a diagnosis of psoriatic arthritis include:
- Psoriasis in the patient, or a family history of psoriasis or psoriatic arthritis.
- A negative test result for Rheumatoid factor, a blood factor associated with rheumatoid arthritis.
- Arthritis symptoms in the distal Interphalangeal articulations of hand (the joints closest to the tips of the fingers). This is not typical of rheumatoid arthritis.
- Ridging or pitting of fingernails or toenails (onycholysis), which is associated with psoriasis and psoriatic arthritis.
- Radiologic images indicating joint change.
Other symptoms that are more typical of psoriatic arthritis than other forms of arthritis include inflammation in the Achilles tendon (at the back of the heel) or the Plantar fascia (bottom of the feet), and dactylitis (sausage-like swelling of the fingers or toes).
Classification
There are five main types of psoriatic arthritis:
- Asymmetric: This type affects around 70% of patients and is generally mild. This type does not occur in the same joints on both sides of the body and usually only involves fewer than 3 joints.
- Symmetric: This type accounts for around 25% of cases, and affects joints on both sides of the body simultaneously. This type is most similar to rheumatoid arthritis and is disabling in around 50% of all cases.
- Arthritis mutilans (M07.1): Affects less than 5% of patients and is a severe, deforming and destructive arthritis. This condition can progress over months or years causing severe joint damage. Arthritis mutilans has also been called chronic absorptive arthritis, and may be seen in rheumatoid arthritis as well.
- Spondylitis (M07.2): This type is characterised by stiffness of the spine or neck, but can also affect the hands and feet, in a similar fashion to symmetric arthritis.
- Distal interphalangeal predominant (M07.0): This type of psoriatic arthritis is found in about 5% of patients, and is characterised by inflammation and stiffness in the joints nearest to the ends of the fingers and toes. Nail changes are often marked.
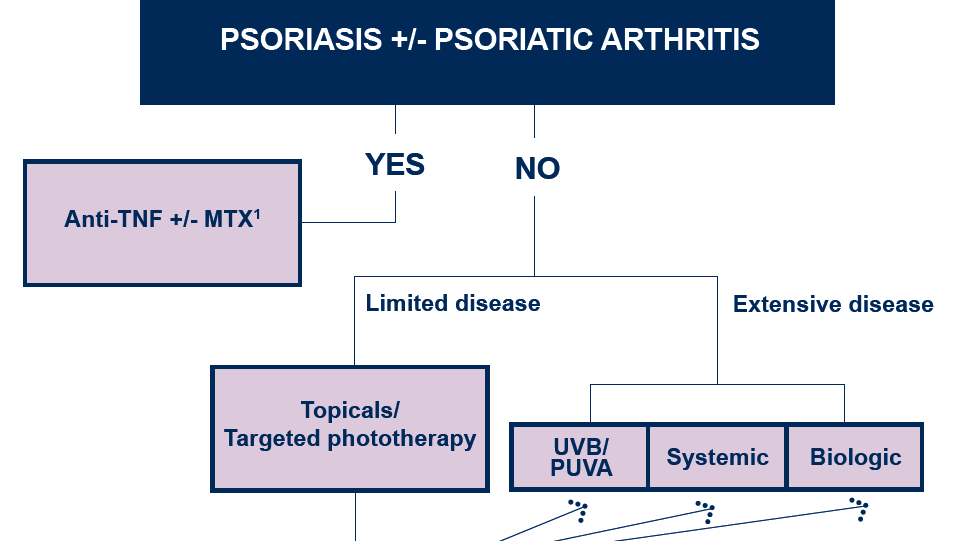
Treatments
The underlying process in psoriatic arthritis is inflammation; therefore, treatments are directed at reducing and controlling inflammation. Milder cases of psoriatic arthitis may be treated with NSAIDS alone; however, there is a trend toward earlier use of disease-modifying antirheumatic drugs or biological response modifiers to prevent irreversible joint destruction.
Nonsteroidal anti-inflammatory drugs
Typically the medications first prescribed for psoriatic arthritis are NSAIDs such as ibuprofen and naproxen followed by more potent NSAIDs like diclofenac, indomethacin, and etodolac. NSAIDs can irritate the stomach and intestine, and long-term use can lead to gastrointestinal bleeding. Other potential adverse effects include damage to the kidneys and cardiovascular system.
Disease-modifying antirheumatic drugs
These are used in persistent symptomatic cases without exacerbation. Rather than just reducing pain and inflammation, this class of drugs helps limit the amount of joint damage that occurs in psoriatic arthritis. Most DMARDs act slowly and may take weeks or even months to take full effect. Drugs such as methotrexate or leflunomide are commonly prescribed; other DMARDS used to treat psoriatic arthritis include cyclosporin, azathioprine, and sulfasalazine. These immunosuppressant drugs can also reduce psoriasis skin symptoms but can lead to liver and kidney problems and an increased risk of serious infection.
Biological response modifiers
Recently, a new class of therapeutics called biological response modifiers or biologics has been developed using recombinant DNA technology. Biologic medications are derived from living cells cultured in a laboratory. Unlike traditional DMARDS that affect the entire immune system, biologics target specific parts of the immune system. They are given by injection or intravenous (IV) infusion.
Biologics prescribed for psoriatic arthritis are TNF-? inhibitors, including infliximab, etanercept, golimumab, certolizumab pegol and adalimumab, as well as the IL-12/IL-23 inhibitor ustekinumab.
Biologics may increase the risk of minor and serious infections. More rarely, they may be associated with nervous system disorders, blood disorders or certain types of cancer.
Other treatments
Retinoid etretinate 30 mg/day is effective for both arthritis and skin lesions. Photochemotherapy with methoxy psoralen and long wave ultraviolet light (PUVA) are used for severe skin lesions. Doctors may use joint injections with corticosteroids in cases where one joint is severely affected. In psoriatic arthritis patients with severe joint damage orthopedic surgery may be implemented to correct joint destruction, usually with use of a joint replacement. Surgery is effective for pain alleviation, correcting joint disfigurement, and reinforcing joint usefulness and strength.
Epidemiology
Seventy percent of people who develop psoriatic arthritis first show signs of psoriasis on the skin, 15 percent develop skin psoriasis and arthritis at the same time, and 15 percent develop skin psoriasis following the onset of psoriatic arthritis.
Psoriatic arthritis can develop in people who have any level severity of psoriatic skin disease from mild to very severe.
Psoriatic arthritis tends to appear about 10 years after the first signs of psoriasis. For the majority of people this is between the ages of 30 and 55, but the disease can also affect children. The onset of psoriatic arthritis symptoms before symptoms of skin psoriasis is more common in children than adults.
More than 80% of patients with psoriatic arthritis will have psoriatic nail lesions characterized by nail pitting, separation of the nail from the underlying nail bed, ridging and cracking, or more extremely, loss of the nail itself (onycholysis).
Men and women are equally affected by this condition. Like psoriasis, psoriatic arthritis is more common among Caucasians than Africans or Asians.
Are You Looking for Products
Here some products related to "Psoriatic Arthritis".
*Organic* Arnica & MSM na..
Hyland's Arthritis Pain F..
Hyland's Arthritis Pain F..
Hyland's Arthritis Pain F..
Get these at Amazon.com* amzn.to is official short URL for Amazon.com, provided by Bitly
Source of the article : here

EmoticonEmoticon